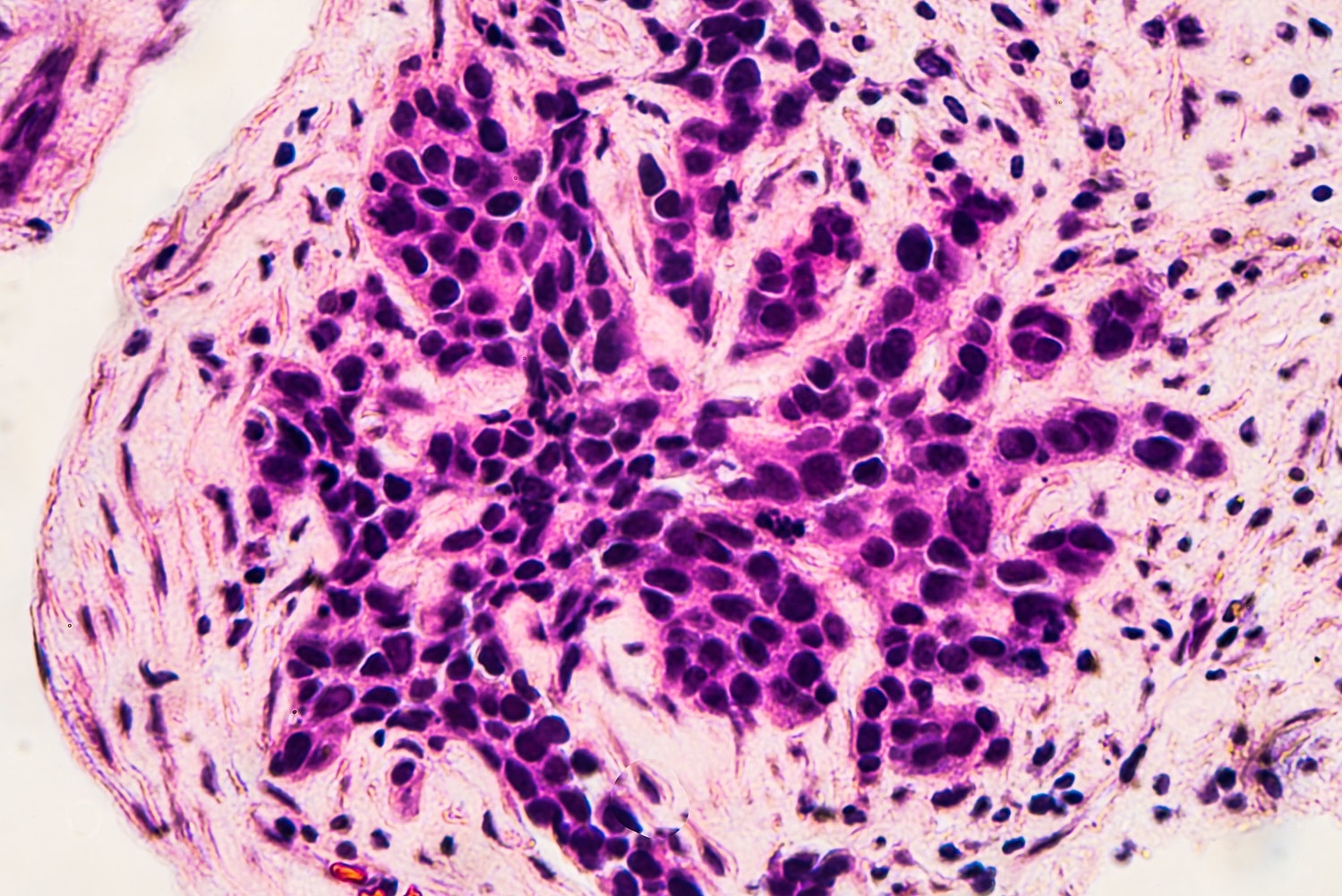
Any type of hormonal contraceptive may increase risk of breast cancer
Thursday 23rd Mar 2023, 10.54am
Previous studies have shown that use of the combined contraceptive pill, which combines oestrogen and progestogen, is associated with a small increase in the risk of developing breast cancer that declines after stopping use. Use of progestogen-only contraceptives has increased substantially in recent years, but information on their association with breast cancer risk was limited. In 2020, there were almost as many prescriptions issued in England for progestogen-only oral contraceptives as there were for combined oral contraceptives.
The researchers analysed data from 9,498 women who developed invasive breast cancer between ages 20 to 49 and 18,171 closely-matched women without breast cancer who acted as controls. The data were collected by the Clinical Practice Research Datalink (CPRD). 44% of women with breast cancer and 39% of women without breast cancer included in the study had a prescription for a hormonal contraceptive an average of three years before diagnosis, around half of whom were last prescribed a progestogen-only contraceptive.
The data were used to calculate the strength of the association between use of each type of hormonal contraceptive and breast cancer risk. These calculations were then adjusted to take into account established risk factors such as body mass index (BMI), number of recorded births, and the time since a woman’s last birth. The researchers combined the CPRD results on oral contraceptive use with those from other previously published studies to estimate absolute excess risks, meaning the additional number of women who would be expected to develop breast cancer in those who used oral contraceptives compared to those who did not.
Key findings:
• In the CPRD data, there was a significant increase in risk of breast cancer associated with hormonal contraceptive use, regardless of whether the contraceptive last prescribed was a combined (oestrogen and progestogen) oral preparation (23%, OR=1.23 95% CI 1.14-1.32), a progestogen-only oral preparation (26%, OR=1.26 95% CI 1.16-1.37), an injected progestogen (25%, OR=1.25 95% CI 1.07-1.45), or a progestogen-releasing intra-uterine device (32%, OR=1.32 95% CI 1.17-1.49);
• In the CPRD data, the increased risk of breast cancer associated with oral contraceptive use declined after stopping use. The increased risks were: last prescribed within the last year (33%, OR=1.33 95% CI 1.23-1.44); last prescribed one-four years ago (17%, OR=1.17 95% CI 1.07-1.29); last prescribed five or more years ago (15%, OR=1.15 95% CI 1.04-1.28);
• When the findings for progestogen-only contraceptives were combined with previously published studies, there was an increased risk of breast cancer in current and recent users of all four types of progestogen-only preparations: oral (29%, OR=1.29, 95% CI 1.21-1.37), injected (18%, OR=1.18, 95% CI 1.07-1.30), implanted (28%, OR=1.28, 95% CI 1.08-1.51), and intra-uterine devices (21%, OR=1.21, 95% CI 1.14-1.28);
• The researchers estimated that the absolute excess risk of developing breast cancer over a 15-year period in women with five years use of oral contraceptives ranged from eight in 100,000 women for use from age 16 to 20, to 265 in 100,000 for use from age 35 to 39.
Kirstin Pirie, statistical programmer at Oxford Population Health, and one of the lead authors, said: ‘The findings suggest that current or recent use of all types of progestogen-only contraceptives is associated with a slight increase in breast cancer risk, similar to that associated with use of combined oral contraceptives. Given that a person’s underlying risk of developing breast cancer increases with advancing age, the absolute excess risk of breast cancer associated with either type of oral contraceptive will be smaller in women who use it at younger ages. These excess risks must, however, be viewed in the context of the well-established benefits of contraceptive use in women’s reproductive years.’
The researchers also note that although these findings provide evidence about the short-term associations between hormonal contraceptives and breast cancer risk, they do not provide information regarding longer-term associations, or the impact of total duration of contraceptive use on breast cancer risk, since information on a woman’s prescription record prior to joining a participating GP practice would not have been available within the CPRD database.
The study, ‘Combined and progestagen-only hormonal contraceptives and breast cancer risk: A UK nested case–control study and meta-analysis‘, can be read in PLOS Medicine.
